Kentucky’s uninsured rate rose to 6.9% in 2024, up from 5.6% in 2023, with most people enrolled in a plan through their employer, Medicaid, Medicare/Medicare Advantage, or the Marketplace (known as kynect in Kentucky). However, coverage isn’t enough. Despite this low uninsured rate, Kentucky continues to rank near the bottom in overall health outcomes. Under a grant from The Commonwealth Fund, The Asclepius Initiative partnered with University of Louisville researchers to talk with insured adults from across the Commonwealth to understand why. Their stories paint a clear picture: health insurance alone isn’t enough to guarantee access to care.
Study Participants
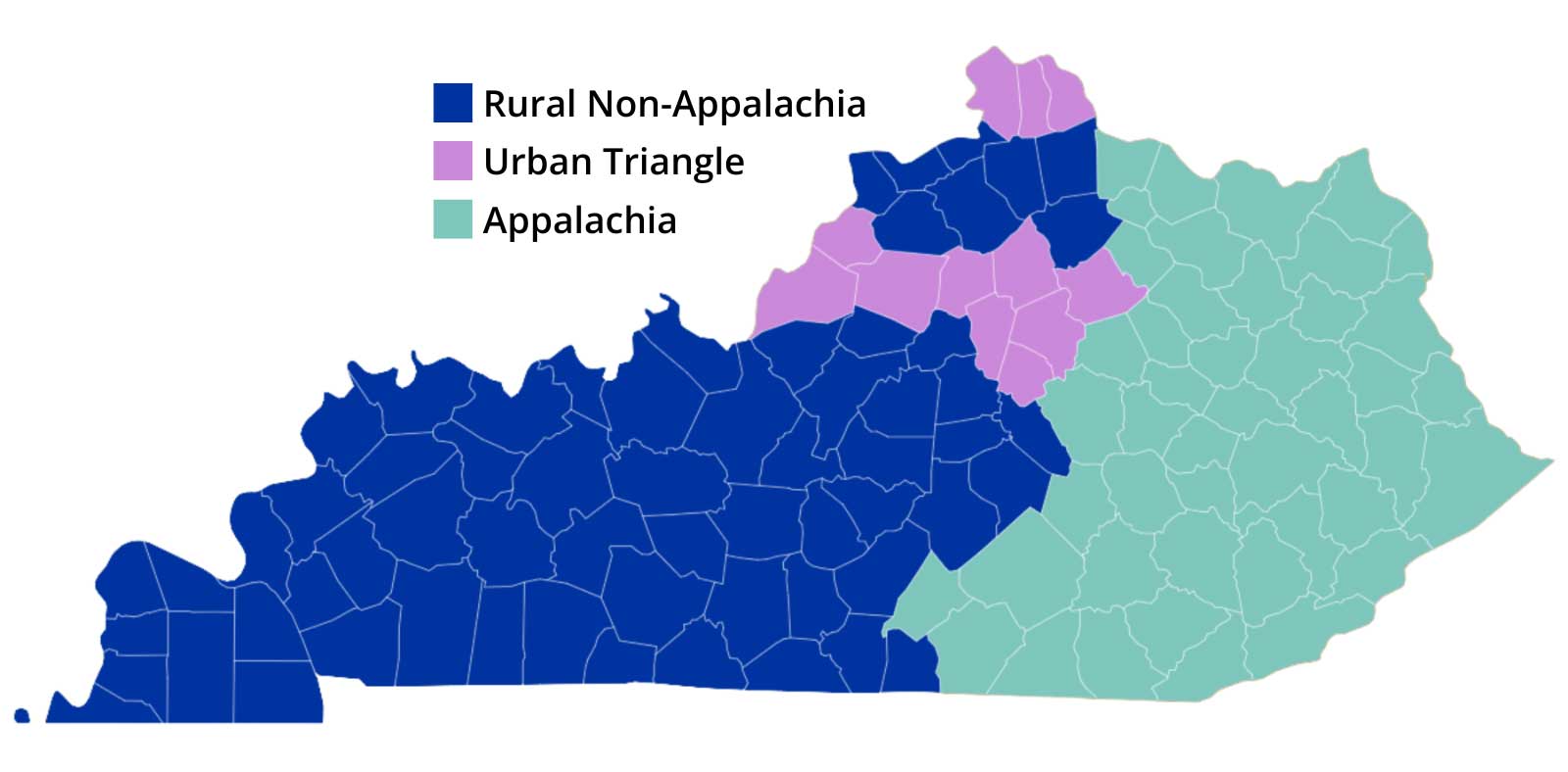
We interviewed 73 people from three regions across the state: Appalachia, non-Appalachian rural Kentucky, and the Urban Triangle (Louisville, Lexington, Frankfort, and Northern Kentucky).
Participants had one of four types of health care coverage: Medicaid, Medicare/Medicare Advantage, Marketplace plans, or employer-sponsored coverage. Ages ranged from 18 to 75, including people with different health needs, income levels, and backgrounds. All interviews were conducted remotely, and each conversation lasted between one and two hours.
Across every part of the state and insurance group, people described obstacles that made getting care difficult, stressful, or simply impossible.
Cost Is Still a Major Barrier
Even though everyone in the study had health care coverage, costs were the number one reason people avoided care. Many talked about high premiums, copays, and deductibles that made routine visits unaffordable. Others worried that the costs would be too much, even if they didn’t know what they were.
One woman with insurance through her job said her copays were so high she had to choose between going to the doctor and buying groceries. Another participant skipped a medically necessary test after she was told she would need to pay $3,000 before the hospital would schedule it. A Medicaid participant told us she wouldn’t get a mammogram to screen for breast cancer because she assumed it would be too expensive, when in reality, the test would have been fully covered without out-of-pocket costs to her.
These concerns reflect a growing national problem. Last week, the Senate rejected a bill that would extend enhanced premium tax credits (ePTCs) for Marketplace coverage. More than 88,000 Kentuckians get their coverage through kynect, Kentucky’s Marketplace, with about 88% getting premium tax credits to make coverage more affordable. Congress’s failure to extend the enhanced premium tax credits means many people who have Marketplace coverage will pay higher premiums for 2026. For some, costs will more than double. While ePTCs only apply to Marketplace plans, the increase in costs is spilling over into employer-sponsored plans as well, since the insurance companies that sell coverage on the Marketplace also provide employer-based coverage.
This reinforces what our study participants told us: having coverage does not guarantee access to care.
Costs Aren’t the Only Barriers to Care
Many study participants noted that it was hard to get appointments, especially with primary care providers, specialists, and dentists. In some rural counties, entire communities rely on only one or two clinics. Many people said they waited months – even a full year – for an appointment. Some had to travel for hours or go out of state to get the care they needed.
Dental care stood out as a serious problem. Many people told us that dentists in their area were not accepting new patients or did not take Medicaid. Tooth loss was so common in some communities that it was “normal.”
Reliable transportation is another barrier to care. Some people told us they don’t have a car; others said that ride services, such as Medicaid transportation, arrived late, failed to return for pickup, or sent vehicles that could not accommodate them. These problems led to missed appointments and lost wages.
Kentuckians also described the emotional and practical toll of dealing with insurance companies. Many said they spent hours on the phone trying to get prior authorizations for treatment or prescriptions approved. Some went weeks without the medications they needed while waiting for a decision. Study participants said these experiences made them feel that the system was designed to benefit insurance companies rather than patients.
What This Tells Us: Health Care Coverage Isn’t Enough in Kentucky
The study makes one thing clear: health coverage opens the door to care, but many Kentuckians still can’t get through it. High costs, provider shortages, long wait times, transportation barriers, insurance rules, and more make it difficult to access care and lead to poorer health outcomes across the state.
Kentucky’s progress in expanding access to health care coverage has made a difference. But to truly improve health, we must address the obstacles that keep people from obtaining coverage or using the coverage they have. Kentuckians need care that is affordable, available, and easy to use. A universal coverage system would reduce many of the challenges our study participants described, so people can focus on their health rather than navigating a complicated, expensive system. Only then can coverage translate into better health.
TAI’s findings have been published by The Commonwealth Fund. Click here to read more.

